10 Ways to Build a Calm and Predictable Residential Care Environment
How can I make my home calmer, safer and more predictable for ND young people?
Managing a crisis in a busy home is exhausting and often feels like fighting a losing battle. You want to support the young people in your care, but constant escalations, sensory overload and unpredictable behaviors make it impossible to find a baseline of safety. You aren't looking for generic parenting advice; you need operational strategies that work in a high-stress residential setting.
Key Takeaways
- Low-arousal environments function by systematically reducing sensory input—noise, light and clutter—to lower the baseline cortisol levels of neurodivergent (ND) residents.
- Predictability cues such as visual schedules and consistent staffing rosters, reduce executive function load by removing the need for residents to constantly process new information.
- SPARK Care™ principles prioritize emotional safety planning over compliance, shifting the focus from managing behavior to preventing dysregulation.
- Co-regulation requires staff to manage their own physiological state first, as dysregulated adults cannot effectively de-escalate a dysregulated child.
- Trauma-informed environment changes focus on physical layout adjustments that eliminate feeling trapped, which directly counters the fight-or-flight response.
The Neuroscience of Stability
Why does a chaotic environment trigger ND meltdowns?
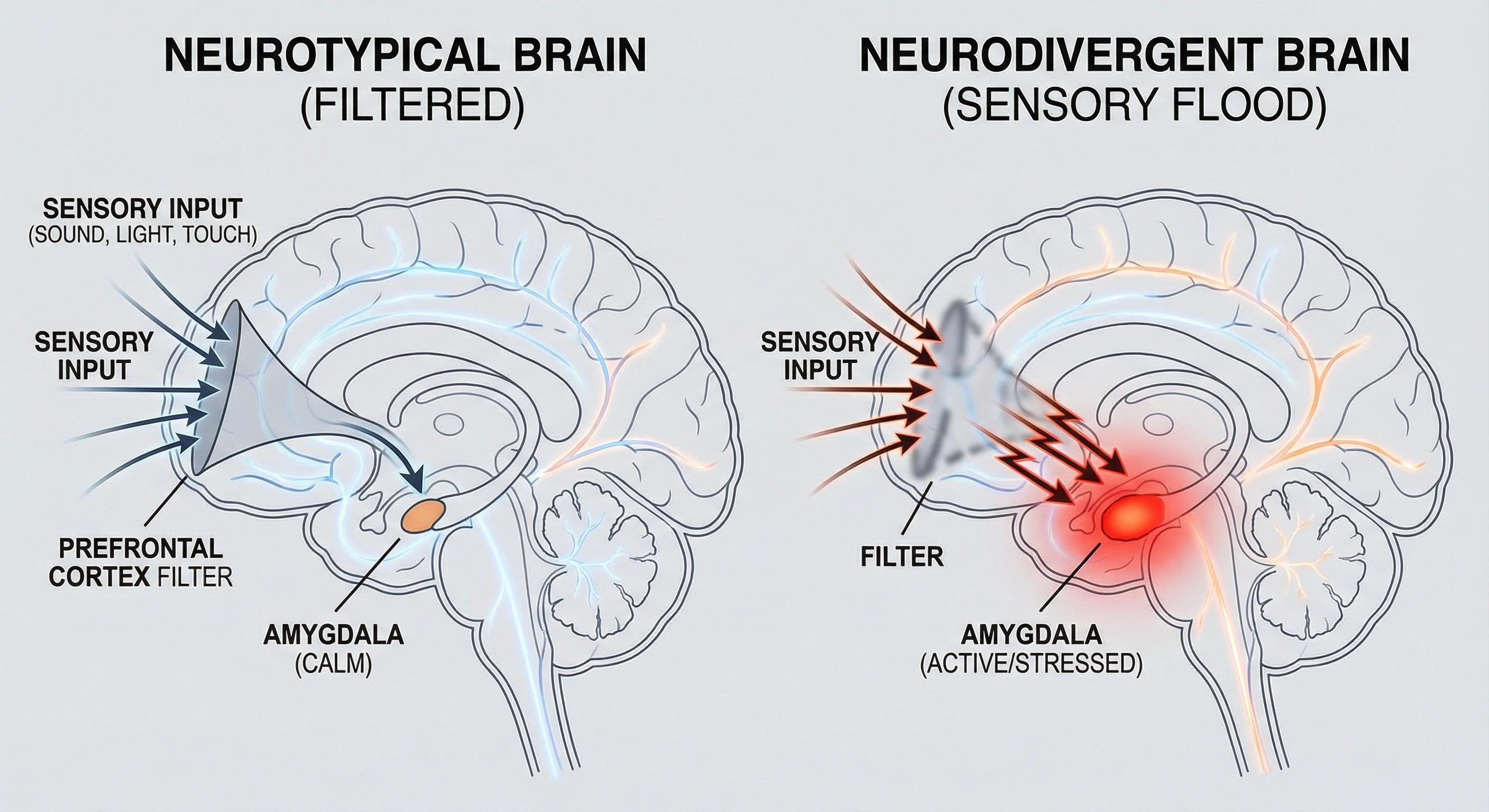
Chaotic environments trigger meltdowns because the neurodivergent brain often lacks the filter to deprioritize irrelevant sensory data, leading to rapid cognitive overload. In a typical brain, background noise or visual clutter is ignored; in an ADHD or autistic brain, every input is processed with equal urgency. This floods the prefrontal cortex and activates the amygdala, shifting the brain into survival mode (fight, flight, or freeze) regardless of actual danger levels. We often see homes that look "tidy" but are sensorially loud, filled with bright patterns or constant radio noise, which keeps residents in a state of hypervigilance.
How do routines improve calm?
Routines improve calm by externalizing executive function, allowing the brain to bypass energy-intensive decision-making processes. When a young person knows exactly what happens next, their brain stops scanning for threats or variables. This predictability reduces the metabolic cost of processing the day, leaving more cognitive energy available for emotional regulation and social interaction. In our experience, "flexible routines" often fail; strict, visual and repetitive structures provide the safety framework required for trauma recovery.
What environment supports ND regulation?
An environment supports ND regulation when it offers "escape hatches" and low-demand zones where sensory input is strictly controlled. This concept, central to the low-arousal care model, involves creating physical spaces where lighting is dimmable, acoustics are dampened and social interaction is optional. This works by allowing the parasympathetic nervous system to engage, bringing the heart rate down and ending the stress cycle. We recommend auditing communal areas to ensure there are always accessible corners or rooms designed solely for decompression, not activity.
Implementing Safety and Structure
How do I reduce chaos at my children's care home?
You reduce chaos by implementing ND-safe routines that eliminate ambiguity from transitions. Chaos in a residential setting is rarely about the volume of people; it's about the unpredictability of their movements and demands. By standardizing shift handovers, meal times and activity blocks, you remove the variables that cause anxiety. This creates a calm and predictable residential care environment where the structure holds the anxiety, so the staff and children don't have to.
Why is emotional safety planning critical?
Emotional safety planning is critical because it shifts the intervention point from "reaction" to "prevention." Traditional risk assessments focus on physical harm, but emotional safety plans map out specific triggers - like sudden loud noises or specific tones of voice - that precede a behavioral escalation. By identifying and removing these antecedents, you stop the biological stress response before it reaches a tipping point. We find that homes using proactive safety planning see a significant reduction in physical interventions.
How to Audit Your Home for Sensory Triggers
- Map the sensory hotspots. Walk through the home at the busiest time of day with a decibel meter and a light meter. Identify areas where noise levels consistently spike or where lighting creates glare, as these are prime locations for dysregulation.
- Strip back the visual noise. Remove 50% of the wall displays, notices and decorations in communal areas. Neurodivergent brains often process visual clutter as tasks to be completed; removing it lowers the cognitive load immediately.
- Zoning the floorplan. Designate specific zones for high energy and low energy using different colored rugs or furniture arrangements. Ensure that "quiet zones" are physically separated from high-traffic transition areas like hallways or kitchens.
FAQs
What is the low-arousal approach?
The low-arousal approach is a behavior management philosophy that focuses on changing the environment and staff behavior to reduce stress, rather than demanding change from the distressed individual. It prioritizes de-escalation and sensory reduction to prevent crisis situations.
How does SPARK Care™ differ from standard care?
SPARK Care™ differs by integrating sensory regulation and trauma-informed principles directly into daily operations. Unlike standard models that may prioritize compliance or behavioral modification, this framework focuses on creating a feeling of safety to enable natural development and healing.
Can you fix a chaotic home without changing staff?
Yes, you can fix a chaotic home without changing staff by changing the systems they use. Implementing strict routines, clear communication protocols and visual schedules forces a structural change that aligns staff behavior, regardless of individual personality types.
Why do "normal" parenting strategies fail in care homes?
"Normal" strategies fail because they assume a neurotypical attachment style and sensory processing system. Residential care involves high-trauma backgrounds and neurodivergence, meaning standard reward-punishment systems often trigger shame or rejection sensitivity rather than improved behavior.
How long does it take to see results from environmental changes?
You typically see results within two weeks of consistent environmental changes. Once the sensory load drops and predictability increases, the residents' baseline stress levels decrease, leading to fewer rapid escalations and better sleep patterns.
Book a strategy audit now to transform chaotic shifts into stable, low-arousal environments that reduce critical incidents and safeguard your staff.
▸ Please note that for your privacy, no data from forms is stored on this website.