Barriers to ND Adaptation in Care Staff: Why It Happens and How to Fix It
The Hidden Cost of Staff Resistance
You can have the best care plans in the file, but they are useless if your floor staff refuse to execute them. Managing a team that clings to "old school" punitive methods while you try to implement trauma-informed care is exhausting. It creates a toxic cycle: the child escalates, staff respond with rigidity, the placement breaks down, and you are left explaining the failure to OFSTED and the LANT. This isn't just about stubbornness or bad attitude. To fix the resistance, you must first understand the psychological and neurological barriers preventing your staff from adapting to neurodiverse needs.
Key Takeaways
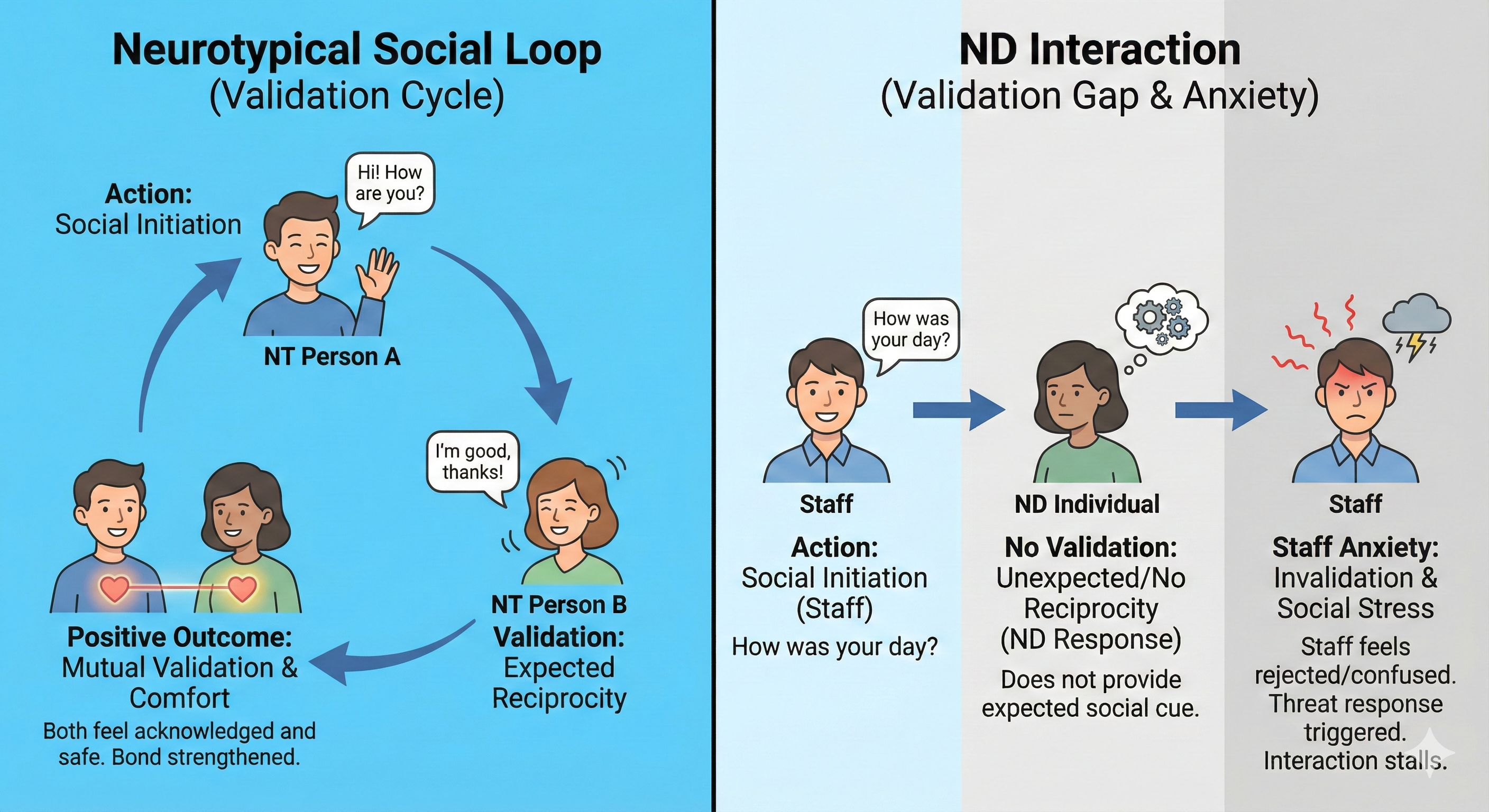
- The Neurotypical Social Expectation Gap: Staff often subconsciously perceive a lack of social reciprocity from ND children (no eye contact, blunt tone) as personal disrespect, triggering a defensive response.
- Cognitive Dissonance in Behaviorism: Shifts to trauma-responsive practice challenge a staff member's core professional identity if they rely heavily on "consequences" and authority for control.
- Fear of Permissiveness: Mindset resistance often stems from the misconception that low-arousal approaches equate to "letting them get away with it," threatening the staff member's sense of order.
- The Cortisol Loop: Stressed staff lose access to their own prefrontal cortex; a dysregulated adult physically cannot access the empathy required for co-regulation.
- SPARK Care Principles: Implementing structured frameworks reduces ambiguity, giving staff a safety net that replaces their reliance on control.
The Psychology of Resistance
Why is ND adaptation difficult for staff?
ND adaptation is difficult because it requires staff to override their innate neurotypical social instincts. Human brains are wired to expect reciprocal social feedback—smiles, compliance, or acknowledgment—to feel safe and respected. When an autistic or ADHD young person does not provide these cues due to their neurology, the staff member’s amygdala interprets this as a social threat or rejection. This triggers a subconscious defense mechanism where the staff member asserts dominance to re-establish their status, leading to power struggles rather than connection.
What causes resistance to trauma responsive practice?
Resistance is primarily caused by the fear of losing control and the invalidation of previous experience. Many veteran support workers built their careers on behaviorist models where compliance was the only metric of success. Introducing trauma responsive practice challenges this foundation by suggesting their previous methods were harmful. To protect their professional ego and avoid the pain of admitting past mistakes, they reject the new framework. They view ND inclusion strategies not as an evolution of care, but as a threat to their competence.
How do mindset gaps impact behaviour interpretation?
Mindset resistance creates a "Fundamental Attribution Error" where staff judge the child's character rather than their state of being. If a staff member lacks knowledge of ND awareness gaps, they attribute a meltdown to being "naughty," "manipulative," or "attention-seeking" (internal character flaws). A trained staff member attributes the same behavior to sensory overload or executive dysfunction (external situational factors). This error changes the intervention from support (co-regulation) to punishment (sanctions), which inevitably escalates the situation.
How to overcome barriers to ND adaptation in care staff
-
Audit the "Unwritten Rules" of the home. Check your culture for hidden rigidity. Explicitly identify and remove "compliance-based" language from handovers. If staff are praised for a "quiet shift" rather than a "regulated shift," you are reinforcing the wrong behaviors.
-
Implement Trauma-Informed Supervision. Move supervision away from task lists and toward reflective practice. Ask staff, "What was happening in your body when he shouted?" rather than "What did you do?" This forces them to recognize their own somatic response and separates their emotional reaction from the child's behavior.
-
Mandate the 'Why' in Incident Reports. Require staff to document the function of the behavior, not just the behavior itself. Refuse to sign off on reports that describe an incident without identifying the antecedent or sensory trigger. This builds the habit of analytical thinking over reactive judgment.
Frequently Asked Questions
Why do staff revert to punitive methods under stress?
Staff revert to punitive methods because high stress (cortisol) shuts down the prefrontal cortex, blocking access to new learning. They default to their oldest, most ingrained neural pathways - usually how they were parented or how they were trained early in their career - which are often authoritarian.
How can training improve understanding of ND needs?
SPARK Care training improves understanding by simulating the sensory and cognitive load of neurodiversity. It moves knowledge from an academic concept to a visceral experience, forcing staff to feel the frustration of a system that doesn't fit their brain, which builds genuine empathy.
Is resistance always a sign of a bad support worker?
No, resistance is often a symptom of burnout or insecurity. A staff member who feels unsafe or unsupported will cling to rigid rules as a survival strategy. addressing the barriers to ND adaptation in care staff often requires supporting the staff member's nervous system first.
What is the biggest barrier to reflective learning?
The biggest barrier is a culture of blame. If staff believe admitting a mistake leads to disciplinary action, they will defend their actions rather than reflect on them. You must create psychological safety where "I got it wrong" is viewed as a learning opportunity, not a failure.
Stop the cycle of staff burnout and placement breakdown by booking a consultation with AshDHD Learning to implement the SPARK Care framework in your home today.
Author Bio
AshDHD Learning is a specialist training provider for the care sector. With deep expertise in SPARK Care principles and trauma informed supervision, we partner with care homes to upskill leadership and frontline staff. Our goal is to close ND awareness gaps and create stable, nurturing environments for neurodiverse young people.
▸ Please note that for your privacy, no data from forms is stored on this website.